Comparison of Anticancer Effects between Platinum Levetiracetam and Platinum Azidothymidine through the Expression of Biomarker Genes on Cancer Cell Lines
-
 Sabokrouh, Abdolreza
Department of Biochemistry, Faculty of Medicine, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran, Tel: +98 9127272170; E-mail: sabokrouh22@gmail.com
Sabokrouh, Abdolreza
Department of Biochemistry, Faculty of Medicine, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran, Tel: +98 9127272170; E-mail: sabokrouh22@gmail.com
-
Ghaffari, Nasim
-
Department of Biochemistry and Biophysics, Faculty of Advanced Sciences and Technology, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran
-
Karimi Tafreshi , Zahra
-
Department of Biochemistry and Biophysics, Faculty of Advanced Sciences and Technology, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran
-
Atabi, Freshteh
-
Department of Biochemistry and Biophysics, Faculty of Advanced Sciences and Technology, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran
-
Sharifi, Zohreh
-
Blood Transfusion Research Center, High institute for Research and Education in Transfusion Medicine, Tehran, Iran
Abstract: Background: The utilization of biomarkers is a way to assess the efficacy of recently created anticancer drugs. MiRNAs, telomerase, and Bcl-2 are extensively utilized as biomarkers for this purpose. This study aims to evaluate the comparison of the newly synthesized platinum compounds such as Platinum Azidothymidine (Pt-AZT) with Platinum Levetiracetam (Pt-Lev) on HepG2 cancer cell lines via the biomarkers.
Methods: In this study, cells were divided into four groups: Group A (HDF cells) were the normal negative control group, group B were HepG2 untreated cancer cells, and groups C and D were treated cancer cells with Pt-AZT and Pt-Lev, respectively. After evaluating the LC50 for the drugs by MTT test, the relative gene expression of the biomarkers was determined by qPCR.
Results: The results showed a significant decrease for antiapoptotic genes including miRNA-21 (5.1±0.014), telomerase (0.56±0.48), Bcl-2 (0.41±0.276) in group D, whereas in group C was more than group D for miRNA-21 (6.0±0.141), telomerase (3.49±0.231), Bcl-2 (4.93±0.276) also there was a significant increase in miRNA-122 (33.97±0.04) in group D, whereas in group C was (28.36±0.007) and so lower than group D. Most of the investigated groups showed a significant difference (p<0.05). In addition, there were widespread apoptotic regions in Pt-Lev treatment compared to Pt-AZT.
Conclusion: The advantages of using Pt-Lev were more powerful anticancer effects on biomarkers through inhibition of antiapoptotic and stimulation proapoptotic factors and also lower side effects and lower drug resistance than Pt-AZT; therefore, it can be considered a more effective anti-cancer therapy.
Introduction :
Cancers are caused by any permanent damage in DNA molecules which can lead to changes in proto-oncogene activity through activating it or by inactivation of tumor suppressor genes. In proto-oncogenes, it can be activated by translocations such as translocation of the c-myc proto-oncogene from chromosome 8 to one of the immunoglobulin loci on chromosomes 2, 14, or 22 resulting in Burkitt's lymphomas, or by point mutation. For example, point mutations of genes coding for guanosine triphosphate-binding proteins, such as H-, K-, or N-ras or G proteins, can be oncogenic as noted in a large variety of malignant neoplasm. Functional loss of "tumor suppressor genes" is found in many tumors such as colon and lung cancers 1. Conventional cancer therapies include surgical resection of the tumors followed by radiotherapy with X-rays and/or chemotherapy. Radiation therapy can damage healthy cells, organs, and tissues 2. Today, a clinical trial is shifting to chemotherapy along with using biomarkers for improvement in cancer treatment 3. The use of biomarkers in the treatment and monitoring of cancer is now common.
Cancer biomarkers are classified into anti-apoptotic biomarkers such as telomerase, Bcl-2, miRNA-21, etc. and their expression is elevated in many cancers 4. Telomerase functions in the maintenance of telomeres and is indispensable for immortalization. Bcl-2 was reported as a direct modulator of telomerase activity 5. MicroRNAs (miRNAs) are small non-coding RNAs with a length of about 19-25 nt, which can regulate various target genes and are thus involved in the regulation of a variety of biological and pathological processes, including the formation and development of cancer 6. Additionally, many studies have shown that miRNAs are involved in the drug resistance of tumor cells 7. Plasma miRNAs including miRNA-21 and miRNA-155 might be potential biomarkers as onco-miR in Human Hepatocellular Carcinoma (HCC) subjects 8. On the other hand, expression of pro-apoptotic biomarkers such as FASLG, BAX, miRNA-122, etc. is reduced in most of the cancers 9.
MiRNA-21 is highly expressed in mammalian cells and functions as an anti-apoptotic and pro-survival factor in various malignancies, including breast, prostate, and liver cancers; thus, it serves as a biomarker for these diseases 10. MiRNA-122 is abundantly expressed in hepatocytes, but barely detectable in primary HCCs, hence it has pro-apoptotic characteristic properties and a tumor suppressor, regulates glutamine metabolism, and plays an important role in lipid homeostasis. It is also known as a sensitive and specific biomarker in hepatocytes in mice and humans 11-14, therefore, it can be used in the diagnosis and monitoring of cancer cells in cell culture.
Platinum-based anticancer drugs, including cisplatin, carboplatin, and oxaliplatin, have been approved worldwide for the treatment of several human cancers. Cisplatin, approved by the FDA in 1978, is one of the most effective chemotherapy drugs for cancers such as lung, ovarian, cervical and breast cancers 15,16. In this study, the anticancer power of two newly synthetic compounds, Platinum Levetiracetam (Pt-Lev) compared to platinum Azidothymidine (Pt-AZT) are evaluated through biomarkers gene expression and widespread apoptotic regions, and therefore their anticancer power for cancer therapy 17,18.
Materials and Methods :
Cell culture: In this study, HepG2 cells were cancer cells that were purchased from the National Center for Genetic and Biological Resources of Iran, and Human Dermal Fibroblast cell lines (HDF) were normal cell lines that were prepared at the Pasteur Institute of Tehran. The culture medium for HepG2 cells was DMEM medium containing bovine fetal serum and 2 mM glutamine, penicillin (100 IU/ml) and streptomycin (100 mg/ml) in an incubator (5%) of CO2 at 37°C and atmospheric humidity.
Classification of studied cells: The studied cells were divided into four groups: groups A (HDF cells) as a normal control group and group B (HepG2) as a negative untreated cancer cell group; groups C and D were HepG2 cancer cells, which were treated with Pt-AZT and Pt-Lev, respectively. miRNA-122, miRNA-21, telomerase and Bcl-2 by real-time PCR (RT-qPCR), were evaluated after determining the LC50 by MTT test.
Drugs for treatment: The completely sterile forms of Pt-AZT and Pt-Lev were synthesized from pure and sterile AZT and Lev, respectively, by the Chemistry Department of the Faculty of Basic Sciences of Razi University of Kermanshah, Iran.
MTT assay: Basis of MTT: MTT assay is based on the reduction of MTT solution, a yellow water-soluble tetrazolium dye, by mitochondrial dehydrogenases, which results in purple formazan crystals. After dissolving crystals in DMSO, color production occurs, which is utilized as an indication of live cells; however, dead cells lack this capacity. The intensity of the created color is evaluated at a wavelength of 540 to 630 nm and is directly proportional to the number of living cells.
MTT procedure: First, the monolayer of HDF and HepG2 cells is trypsinized separately to obtain a uniform suspension of the mentioned cells with the desired density, and considering that the primary concentration in the study which was 100 cells/µl to determine the volume of the solution to be added in each well, for obtaining 10,000 cells, the formula X=10000C, was used. In this formula, X represents the volume of solution used in each well and C is primary concentration of stock solution. It incubated the drugs with doses of 100, 200, 400, and 800 µg/ml of Pt-Lev and Pt-AZT at times of 24, 48, 72 hr. Then the supernatant liquid in each well was discarded and 60 µl of MTT solution were added. After incubating for 3-4 hr, by removing the supernatant solution and adding DMSO for dissolution, purple formazon crystals were formed. Using the Nanodrop at 570-620 nm, absorbance was read and LC50 was obtained.
Histopathological experiment: HDF and HepG2 cells in a 25T flask and for 24-48 hr with buffered formalin (10:1) were fixed. Dehydration was done with 90% ethanol, and cleaning with xylene was performed for one hr. The cells were mixed with paraffin wax and cooled by cryogenic plates. Finally, by a microtome, it was cut to obtain 5 μm slides, and with 10 µl of trypan blue solution, each slide was stained.
Molecular study: Levels of molecular study were carried out as follows:
RNA extraction: RNA was extracted from cell culture using a commercially available kit (QIAzol Lysis Reagent) (Qiagen, Frankfurt, Germany).
cDNA synthesis of extracted RNA: cDNA was synthesized using a commercially available kit (Transcriptor First Strand cDNA Synthesis Kit, Roche, Bavaria, Germany). The protocol was according to the kit’s manufacturer.
Real-time PCR for the study of the quantity of gene expressions: Real-time quantitative PCRs were performed by an ABI 7500 Real-Time PCR System (Applied Biosystems Company, California, USA), utilizing Taqman reagents (Applied Biosystems Company, California, USA) according to the manufacturer’s instructions. The sequences of the oligonucleotides used in PCR amplification of miRNA-21, miRNA-122, and RNU6 (a housekeeping gene as a reference gene) and telomerase, Bcl-2, and β-actin (a housekeeping gene as a reference gene) are shown in table1. The Δct of target genes was obtained by subtracting the threshold cycle (ct) of target genes from those of RNU6 for miRNAs as an endogenous control and also by subtracting the threshold cycle (ct) of target genes from those of β-actin for telomerase, and Bcl-2 was calculated for each group separately. Then, by subtracting the Δct of target genes from the Δct of the control group, ΔΔct was calculated. The fold change of the target gene was estimated by using the following formula: fold change of target gene=2-ΔΔct.
Statistical analysis: Statistical analyses were obtained with the use of SPSS version 26. A p<0.05 was considered significant. A one-way variance test was used for data analysis, and Tukey’s post hoc test was used for pairwise comparisons between the groups.
Results :
MTT results: The MTT test results using the LC50 method demonstrated that at concentrations of 0, 100, 200, 400, and 800 μg/ml Pt-AZT or Pt-Lev on HepG2 cell lines at three times of 24, 48, and 72 hr, there was fifty percent survival of cells at a concentration of 400 μg/ml for Pt-AZT and 200 μg/ml Pt-Lev in 48 and 72 hr, respectively. At zero concentrations of Pt-AZT and Pt-Lev, all of the HepG2 cancer cells were fully viable, but at higher concentrations of Pt-AZT and Pt-Lev, many of the HepG2 cells were killed by apoptosis. The results of MTT tests are displayed in figures 1 and 2, and Pt-Lev showed slight necrosis effects in 800 µg/ml concentrations at 48 and 72 hr, while Pt-AZT showed more necrosis effects than Pt-Lev at the same concentrations and times. Additionally, Pt-Lev and Pt-AZT had no effects on HDF cells in 0, 200, and 400 µg/ml concentrations.
Histopathological results: In this study, group B included untreated cancer cells with several enlarged nuclei, which showed a phase of synthesis in the cell cycle of hepatocytes. There were no apoptotic regions in the cells (Figure 3). In groups C and D, there were several apoptotic regions, but the extension of apoptosis in the Pt-AZT treatment was less compared to the treated cells with Pt-Lev (Figures 4 and 5).
Gene expression results: Th results of the study in group C showed the expression of anti-apoptotic genes such as miRNA-21 (6.0±0.141), telomerase (3.49±0.231), and Bcl-2 (4.93±0.276) was higher than the factors mentioned in Group D, including miRNA-21 (5.10±0.014), telomerase (0.56±0.480), and Bcl-2 (0.41±0.276). On the other hand, in group C, the expression of proapoptotic factor miRNA-122 (28.36±0.007) was lower than the mentioned gene expression in group D (33.97±0.04). Proapoptotic genes, including miRNA-122 (1.12± 0.014), exhibited high expression levels in group B (untreated cancer group). In contrast, antiapoptotic genes such as miRNA-21 (8.65±0.07), telomerase (5.16±5.08), and Bcl-2 (9.40±11.6) demonstrated significantly elevated expression levels. The three antiapoptotic genes previously mentioned—telomerase (0.36±0.252), Bcl-2 (0.32±0.23), and miRNA-21 (0.11±0.007)—along with the proapoptotic gene miRNA-122 (9.12±0.01), exhibited markedly low expression levels in group A, the healthy control group. Figure 6 makes it simple to see these circumstances. Significant differences were seen between the group majorities (p<0.05) (Figure 6, Table 2).
Discussion :
In this study, the anticancer effects of Pt-AZT and Pt-Lev were evaluated by the expression levels of miRNAs, including miRNA-21 and miRNA-122, and telomerase and Bcl-2 in four studied groups. The study findings showed that in group D (the cancer-treated group with Pt-Lev), the expression of antiapoptotic factors including miRNA-21, telomerase, and Bcl-2 was lower than in group C (the cancer-treated group with Pt-AZT), and a proapoptotic factor, miRNA-122, was higher than in group C.
Several studies have demonstrated the anti-tumor potential of nucleoside analogs. Among these compounds, zidovudine, or Azidothymidine (AZT), which is a thymidine analogue, can inhibit DNA polymerase (AZT-5'-triphosphate), blocking the elongation of the DNA strand due to the absence of a 3'-hydroxyl group, causing a reduction in telomerase activity and consequently senescence and death of tumor cells 19,20. Lev in Pt-Lev is an antiepileptic drug that by more inhibiting previously mentioned antiapoptotic factors i.e., telomerase, Bcl-2, miRNA-21, and more stimulating proapoptotic factors i.e., miRNA-122 has more anti-cancer power than Pt-AZT. The apoptotic regions in Pt-Lev were more extensive than in Pt-AZT. However, it seems platinum components of Pt-AZT and Pt-Lev have the same effects as follows:
Excessive uptake of platinum compounds by the genome of cancer cells, particularly through binding to the organic base guanine, results in the formation of adducts, especially 1,3-intrastrand guanine crosslinks. These adducts are resistant to repair, ultimately leading to apoptosis of the cancer cells. Platinum-based compounds demonstrate stronger anticancer effects compared to their non-platinum counterparts 17,21.
Some research supports this opinion. For example, while treating tumor cells with cisplatin, carboplatin, and oxaliplatin, it was discovered that cisplatin often enters tumor cells via Copper Transporter 1 (CTR1). The activation stage of the platinum complex involves the substitution of the chloro-ligand(s) by water molecules or other small molecules that contain sulfhydryl groups once it has entered the tumor cell. Following a sequence of chemical events within the cytoplasm, platinum forms intra- and inter-stranded crosslinks with DNA, altering its structure and causing damage to the molecule. The most nucleophilic DNA location is guanine's N7 position, which is preferentially plastinated and exposed in the main groove. The damage to DNA can stop the cell cycle and cause apoptosis in tumor cells that are growing quickly. Many studies revealed that platinum compounds had more anticancer effects than original drugs.
In a study, it was shown that the anticancer effects of Pt-AZT on the liver of live rats were greater than AZT due to more inhibition of telomerase and Bcl-2 by Pt-AZT than AZT 22. In a study, it was shown that Pt-Lev had more anticancer effects than Lev by decreasing miRNA-21, telomerase, and Bcl-2 and increasing FASLG when HepG2 cell lines were treated with Pt-Lev and Lev 23. In a study, the anti-cancer effects of cisplatin were associated with a down-regulation of miRNA-21 expression and an up-regulation of miRNA-122 24. In another study, it was shown that carboplatin may up-regulate SMAD7 through suppression of miRNA-21 to inhibit TGFβ receptor signaling-mediated Non Small Cell Lung Cancer (NSCLC) invasion 25. In a study, miRNAs have been used as a potential biomarker for early detection of HCC combined with Vascular Endothelial Growth Factor (VEGF) and α Fetoprotein (α-FP) 26. Early-stage HCC is difficult to diagnose; using these biomarkers would likely improve the patients' prognoses. However, as was noted in some studies, using these miRNAs has strong potential to serve as novel biomarkers for the prognosis of some cancers, such as HCC, but not specifically for HCC 27,28.
However, one benefit of using the newly synthesized Pt-Lev compared to Pt-AZT is that it has low side effects, which can be observed in HDF-healthy cell lines treated with Pt-Lev compared to Pt-AZT. Pt-Lev only causes mild necrosis in healthy cells when it is at a high concentration (800 mg/µl) at 48 and 72 hr, but Pt-AZT had significant necrosis at the same concentration and times (800 mg/µl) (Figure 4). Drug resistance in cancer treated cells is created in different ways. One of these methods is via Multidrug Resistance (MDR) regulation by biomarkers; so that antiapoptotic factors such as miRNA-21, telomerase, and Bcl-2 stimulate MDR expression via the Wnt/βcatenin pathway and enhance drug resistance. Also, pro-apoptotic factors such as miRNA-122 inhibit MDR expression via Wnt/βcatenin pathway and enhancing sensitivity to drugs. In this study, Pt-Lev, compared to Pt-AZT showed lower expression of miRNA-21, telomerase, and Bcl-2 (antiapoptotic factors) and higher expression of miRNA-122 (a proapoptotic factor); and therefore, has important roles in decreasing drug resistance compared to Pt-AZT. A study confirmed the view of the present study. According to Cao et al, HCC cells that were not treated showed down-regulation of miR-122; however, up-regulation of miRNA-122 or suppression of Wnt/β-catenin signaling induced HCC cell death and made the cells more susceptible to Oxaliplatin (OXA). Put differently, by suppressing the Wnt/β-catenin pathway, miRNA-122 decreases MDR1 expression and increases HCC's susceptibility to OXA 29.
MicroRNAs are small, noncoding RNAs that play an important role in regulating gene expression at a post-transcriptional level 30. In the present study, results were obtained by treatments via Pt-Lev and Pt-AZT. The results of the present study indicated that in group D miRNA-21 gene expression was lower than the mentioned gene in group C, and for miRNA-122 in the mentioned groups, it was reversed, so that the gene expression for the gene in group D was higher than group C. A point that should be paid attention to in the mentioned groups was the reversal relationship between gene expression of miRNA-21 and miRNA-122 in each of the group’s C and D. The likely reasons for the reverse relation are as follows: It was determined that miRNA-122 directly inhibits the production of cell survival oncomiR miR-21 at the post-transcriptional level, hence promoting apoptosis in HepG2 cells. Nevertheless, it was discovered that miRNA-122 is highly expressed in the primary nucleus of normal HDF cells and is easily localized to the cytoplasm. The nuclear localization of miRNA-122 is markedly diminished in transformed cells, specifically HepG2 cancer cells. The reduced levels of miRNA-122 in the cytoplasm of these cancer cells correlate with an increase in miRNA-21, contributing to the resistance of HepG2 cells to various therapeutic agents. The platinum component of Pt-AZT induces apoptosis in HepG2 cancer cells, leading to an increase in cytoplasmic miRNA-122 through cell membrane rupture, which facilitates nuclear localization. According to a study, miR-122 is highly expressed in the nucleus of original liver cells, but in transformed cells especially in chemoresistant tumor cells—its nuclear localization is noticeably reduced. In HCC tissues and cells, miRNA profiling and RT-qPCR demonstrate an inverse relationship between miR-122 and miR-21; elevating or lowering the nuclear level of miR-122, respectively, decreases or increases the expression of miR-21 29. It appears that the maturation of miRNA-21 is suppressed by miRNA-122's increased nuclear localization. In the present study, the expression of additional biomarkers, such as telomerase and Bcl-2, which are antiapoptotic factors, was reduced in both groups C and D, but the amount of this decrease was greater in group D. Telomerase expression is high in cancer HepG2 cells and low in treated cancer cells, causing apoptosis due to telomere shortening in these cells. Similarly, Bcl-2 expression is decreased in cancer-treated cells, inducing apoptosis and destroying cancer cells.
Conclusion :
The present study findings showed that in group D (the cancer-treated group with Pt-Lev), the expression of antiapoptotic factors including miRNA-21, telomerase, and Bcl-2 was lower than in group C (the cancer-treated group with Pt-AZT), and a proapoptotic factor, miRNA-122, was higher than in group C. The two previously mentioned drugs utilize platinum components to enhance their anticancer effects through the formation of DNA adducts, particularly 1,3 intrastrand purine base adducts, which are irreparable and result in apoptosis. AZT which is a thymidine analogue, can inhibit DNA polymerase (AZT-5'-triphosphate), blocking the elongation of the DNA strand due to the absence of a 3'-hydroxyl group, causing a reduction in telomerase activity and consequently senescence and death of tumor cells. Also Lev as an antiepileptic drug exerts anticancer effects via inhibition antiapoptotic and stimulates proapoptotic factors.
From the above study, it was concluded that the newly synthesized compound, namely Pt-Lev, is a stronger compound for cancer chemotherapy than Pt-AZT due to its stronger effects on biomarkers such as miRNA-21, miRNA-122, telomerase, and Bcl-2. It also increases the extent of apoptosis in cancer cell lines more than the Pt-AZT drug. The advantages of using the newly synthesized Pt-Lev compound were lower side effects by reduction necrosis and lower drug resistance than Pt-AZT; therefore, it can be considered a more effective anti-cancer therapy in cell lines.
Ethical Statement :
This study was performed in line with the principles of the Declaration of Helsinki and ethically approved and was granted by department of Biochemistry and Biophysics, Faculty of Advanced Sciences and Technology, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran (IR.IAU.PS.REC.1399.055).
Acknowledgement :
Funding: The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Conflict of Interest :
The authors declare no conflict of interest.

Figure 1. Biomarkers gene expression in four studied groups.
|
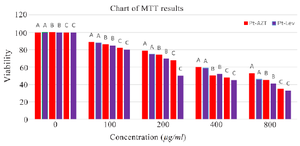
Figure 2. Results of MTT test at different concentrations of drugs. The results showed that LC50 for Pt-AZT was at concentration 400 µg/ml in 48 hr and for Pt-Lev was 200 µg/ml in 72 hr.
- A) 24 hr treatment, B) 48 hr treatment, C) 72 hr
|
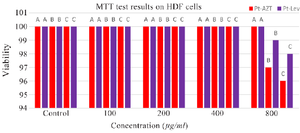
Figure 3. Results of MTT test at different concentrations of drugs on HDF cell lines. The results showed that none of cells underwent apoptosis but there was slight necrosis in 800 µg/ml concentrations of drugs.
- A) 24 hr treatment, B) 48 hr treatment, C) 72 hr
|
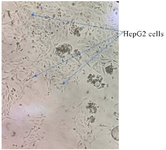
Figure 4. The HepG2 cells before drugs treatments.
|
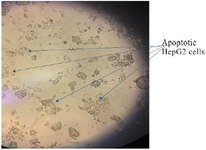
Figure 5. Pt-AZT treatment of HepG2 cells, there were a few apoptotic regions was seen.
|
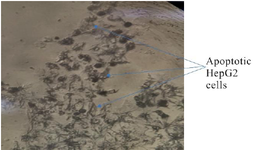
Figure 6. Pt-Lev treatment of HepG2 cells, there were extensive apoptotic regions after treatment.
|
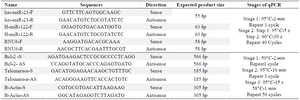
Table. 1 Primers of target genes in sense and antisense with qPCR conditions
|
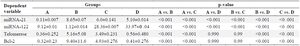
Table 2. Comparative statistical results of miRNA21 and miRNA122 Telomerase and Bcl-2 genes expression in the four studied groups
- Control group, B) Untreated cancer group, C) Cancer group treated with Pt- AZT, D) Cancer group treated with Pt-Lev.
|
|