Association of Catechol-O-Methyl-Transferase and Estrogen Receptors Polymorphism with Severity of Temporomandibular Disorder in Iranian Patients
-
Roudgari, Hassan
-
Genomic Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran
-
Department of Applied Medicine, School of Medicine, Polwarth Building, Foresterhill Health Campus, Aberdeen University, Aberdeen, UK
-
Najafi, Shamsolmoulouk
-
Department of Oral Medicine, Dental Research Center, School of Dentistry, Tehran University of Medical Science, Tehran, Iran
-
Khalilian , Sheyda
-
Department of Medical Genetics, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
-
Ghafarzadeh, Zahra
-
School of Dentistry, Tehran University of Medical Science, Tehran, Iran
-
Hahakzadeh, Aida
-
School of Dentistry, Tehran University of Medical Science, Tehran, Iran
-
Behazin, Sheida
-
School of Dentistry, Tehran University of Medical Science, Tehran, Iran
-
 Sheykhbahaei, Nafiseh
Department of Oral Medicine, Dental Research Center, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran, Tel: +98 9128090967; Fax: +98 21 81633501; E-mail: dsheykhbahaei@gmail.com, nsheykhbahaei@sina.tums.ac.ir
Sheykhbahaei, Nafiseh
Department of Oral Medicine, Dental Research Center, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran, Tel: +98 9128090967; Fax: +98 21 81633501; E-mail: dsheykhbahaei@gmail.com, nsheykhbahaei@sina.tums.ac.ir
Abstract: Background: There are many studies which strongly suggest that the pathophysiology of Temporomandibular joint Disorder (TMD) may also be influenced by genetic conditions. The current study was aimed to evaluate the hypothesis that the polymorphism of estrogen receptor genes, estrogen receptor 1 and 2 (ESR1 and ESR2), and the gene Catechol -O-Methyl-Transferase (COMT) could be Predisposing factor for TMD.
Methods: In this case-control study, blood sample were taken from 100 TMD diagnosed patients based on Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) and 103 healthy individuals as the control group. Tetra ARMS-PCR method was used to amplify and identify COMT rs4680, ESR1 rs1643821, and ESR2 rs1676303 gene polymorphism.
Results: ESR1 genotype AA and GA showed significantly increase probability (OR= 4.80, OR=2.98, respectively) of TMD. ESR2 T/T homozygosity was associated with decreased risk for TMD (OR=0.41). The relationship between COMT and TMD was not statistically significant (p>00.05). The relationship between the severity of TMD and ESR1 was significant (p=0.003). According to the inheritance pattern the COMT and ESR1 gene, in the dominant pattern can be susceptible to TMD and in ESR2 gene, in the recessive pattern can be protective to TMD.
Conclusion: It seems that SNPs of ESR1 rs1643821 has a susceptible role and ESR2 rs1676303 has a protective role against TMD. Also, we add evidences that various genotype of COMT rs4680 were not statistically different between case and control, but allele A in the dominant inherence pattern can be susceptible to TMD.
Introduction :
Temporomandibular joint disorder (TMD) is the most common cause of facial pain and influenced by psychosocial factors (such as stress, anxiety, and somatization) 1, parafunction 2, and genetic risk factor 3. Nowadays, there are debates about the role of genetic variation in the onset of TMD and related pain. There have been many studies on the relationship between genetic polymorphisms and musculoskeletal conditions, which strongly suggest that the pathophysiology of TMD may also be influenced by genetic conditions 4.
There are some genes, mostly related to catecholamine, which are believed to be associated with the regulation of the nociceptive processes, such as the Catechol-O-Methyl-Transferase (COMT) gene 5. The COMT gene is associated with genetic variants 6 and located on the long arm of chromosome 22 and encodes an enzyme that is highly expressed in the central nervous system 7. COMT is highly polymorphic within its coding and non-coding regions, which renders it to produce various forms of COMT enzyme 8. Therefore, COMT Single-Nucleotide Polymorphisms (SNPs) can be somehow used as biomarkers for clinical purposes 9. A functional SNP of the COMT gene results in a valine to methionine mutation at position 158 rs4680 6. Hence, most studies associated with the COMT gene have focused on the rs4680. Overall, rs4680 was associated with psychosocial factors and pain and reduces the activity of blood cell and tissue enzymes by 25-40% 10.
Since the prevalence of TMD was higher in women than men 11, many studies have examined the role of gender in the onset of TMD by examining sex hormones such as estrogen 12,13. Estrogens function is handled by multiple traditional genomic mechanisms that under specific circumstances interact with each other. The genomic mechanisms start by binding of 17α-estradiol to Estrogen Receptor alpha (ERα) (ESR1) or 17β-estradiol to Estrogen Receptor beta (ERβ) (ESR2), these classical receptors are coded by the ESR1 (6q25.1) and ESR2 (14q23.2) genes, respectively. Estrogen receptors as a transcription factor directly affect the specific promoter sequences known as Estrogen Response Elements (ESREs); these specific sequences are the regulatory region of target genes 14. Scientists have identified ESREs in the COMT genes, which are regulated by estrogen receptors 15,16.
Several studies have examined different polymorphisms of estrogen receptor and COMT genes separately 3,17,18, although it seems that the assessment of these three genes has not been performed together in TMD patients, especially in Iranians. The current study aimed to evaluate the hypothesis that the polymorphism of estrogen receptor genes, ESR1 and ESR2, and the gene COMT (regulated by estrogen receptors) could be predisposing factors for TMD.
Materials and Methods :
The study protocol was approved by the Medical Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.DENTISTRY.REC.1397.056). Written informed consent was obtained from all participants.
Case-control study: We conducted a case-control study with two groups of subjects: 100 TMD patients and 103 healthy individuals of the same population. The participants were selected over 6 months between October 2019 and April 2020 randomly. According to Furquim, et al 19 and considering the significance level of 5% and a power of 80%, the sample size was calculated with 76 and 91% of the dominant allele in the control and case groups, respectively. Therefore, the minimum sample size required for each group was 93 participants.
One calibrated investigator evaluated all of the participants clinically by Axis 1 tool of the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) that has been validated for clinical diagnosis of TMD 20. Furthermore, psychosocial impairment and pain-related factors in TMD patients were evaluated using axis II of RDC/TMD, and the severity of TMD was measured by the HELKIMO index 21,22.
Finally, 100 patients including 23 men and 77 women with a mean age of 36 years (18-65 years) as the case group, and a total of 103 age and gender-matched healthy individuals including 38 men and 65 women with a mean age of 35 years (20-54 years) entered the study. All individuals with TMD were selected from the referrals to the Department of Oral and Maxillofacial Diseases and Pain, Faculty of Dentistry, Tehran University of Medical Sciences. The finding of clinical examination of patients with TMD is shown in table 1.
The inclusion criteria were patients with confirmed TMD according to RDC/TMD and signing the informed consent form. Patients with a diagnosis of systemic joint diseases such as rheumatoid arthritis, systemic lupus erythematosus, fibromyalgia, patients with a history of surgery in the orofacial region and/or trauma, pregnant or nursing women and significant medical conditions such as diabetes, cardiovascular diseases or cancer were excluded. Then, with a syringe 5 ml venous blood samples was taken from the antecubital vein. For separation of the hematocrit from the plasma the centrifuge was done at 2000 rpm for 10 min. Blood samples in special tubes containing 3% citric acid were stored at -20°C and within 2 hr sent to a laboratory.
Genotyping: Tetra ARMS-Polymerase Chain Reaction (T-ARMS-PCR) method with specific internal and external primers was used to amplify and identify COMT gene polymorphism rs4680, ESR1 rs1643821, and ESR2 rs1676303 (Table 2). The PCR reaction was performed in a final volume of 25 μl (including 12.5 μl PCR master mix, 0.5 μl of each of the primers, 2.2 M betaine, 2 μl of DNA sample, and 7 μl of distilled water) using ABI VERRITI thermocycler. The application used cycles of denaturation starting at 95°C for 5 min, followed by 10 cycles of 95°C for 30 s, then 63°C for 35 s and 72°C for 45 s plus 20 cycles of 95°C for 30 s. 10 µl of PCR product was electrophoresed on 2% agarose to detect the genotype (Figure 1). After all, a UV transilluminator was used for gel analysis.
Statistical analysis: Descriptive statistics and frequency counts were calculated. Chi-square and Fisher's exact tests were used to determine the association between categorical variables. The Shapiro-Wilk was used to check normality. If the variables were normal, a t-test and Analysis of Variance (ANOVA) were used, and if the variables were not normal, Mann-Whitney and Kruskal-Wallis tests were used to examine the differences between the groups. The association of gene variants was determined by calculating the Odds Ratio (ORs) and their 95% Confidence Interval (CI). All analyses were performed using STATA version 14. A p-value <0.05 was considered as the threshold of rejection area in all analyses and all reported p-values were two-sided.
Results :
The genotype frequencies of COMT SNP rs4680, ESR1 SNP rs1643821, and ESR2 SNP rs1676303 in the TMD and healthy participants are shown in table 3. Our results suggest that there was no significant relationship between COMT rs4680 and TMD (p>0.05). Although the heterozygous GA genotype increased the risk of TMD compared to the wild-type GG genotype, this relationship was not significant (OR=4.67, 95%CI: 0.92 to 45.43; p=0.058). This relationship is also seen between AA homozygous and GG wild-type genotypes (OR=4.78, 95%CI: 0.78 to 50.42; p=0.081). In estrogen receptors, there was a significant relationship between ESR1 rs1643821 and TMD in comparison with the control group. Accordingly, patients with ESR1 rs1643821 genotype AA and GA showed an increased probability (OR=4.80, 95% CI: 1.35, 17.62; p=0.005 and OR=2.98, 1.35, 6.88; p=0.003, respectively) of developing TMD about genotype GG. However, there was no significant relationship between ESR2 rs1676303 heterozygous CT genotype and increased risk of TMD compared to wild type CC genotype, but this relationship was significant between homozygous TT genotype and decreased the risk of TMD compared to wild type CC genotype (OR=0.41, 95%CI: 0.16 to 1.02; p=0.034).
Association of rs4680, rs1643821, and rs1676303 with severity of TMD: Table 4 shows the relationship between the severity of TMD and COMT SNP rs4680, ESR1 SNP rs1643821, and ESR2 SNP rs1676303 in TMD (mild, moderate, and severe) and healthy (normal) groups. According to this table, there was no significant relationship between the severity of TMD and COMT SNP rs4680 (p=0.673) and ESR2 SNP rs1676303 (p=0.189), but the relationship between the severity of TMD and ESR1 SNP rs1643821 was significant (p=0.003).
Association of the severity of TMD with risk factors in TMD patients: From a total of 100 TMD patients, 21 (21%) were male and 79 (79%) were female with a mean age of 35.75 (SD=9.09). Of these, 26 (26%), 10 (10%), and 27 (27%) had severe depression, anxiety, and somatization, respectively. Also 34 (34%), 39 (39%), 51 (51%), and 61 (61%) had pain in Temporomandibular Joint (TMJ), pain in temporalis, pain in the masseter, and pain in TMJ with open mouth, respectively. There was no statistically significant difference between the severity of TMD and age, sex, anxiety, and pain in temporalis (p>0.05), but there was a significant difference between the severity of TMD and depression (p=0.029), pain in TMJ (p=0.03), pain in masseter (p=0.004), and pain in TMJ with mouth opening. There was also a trend between the severity of TMD and somatization. In total, approximately 75.44% of patients in the severe TMD group suffered from TMJ pain during mouth opening (p<0.001) and more than 42.11% of patients with pain in TMJ suffered from severe TMD (p=0.03). More details are provided in table 5.
Also, the inheritance pattern for the alleles of each gene was investigated. Accordingly, in the COMT gene, allele A in the dominant pattern (G/A-A/A), can be susceptible to TMD (p=0/034, OR=4/69). In the ESR1 gene, allele A in the dominant pattern (G/A- A/A), can be susceptible to TMD (p=0/044, OR=1/96) and in the ESR2 gene, allele C in the recessive pattern (C/C-T/C), can be protective to TMD (p =0/03, OR=0/52) (Table 3).
Discussion :
The authors in the present study hypothesized that SNPs at the estrogen receptor genes ESR1 and ESR2 which are functional genes implicated in pain, and also at genes whose expression is regulated by estrogen receptors, such as COMT, are associated with TMD. In the current study, we did not identify any significant association between COMT and the diagnosis of TMD. While there was a significant association between ESR1 rs1643821 and the mutant (TT) genotype of ESR2 with TMD. According to the inheritance pattern the COMT and ESR1 gene, in the dominant pattern can be susceptible to TMD and the ESR2 gene, in the recessive pattern, can be protective against TMD. Consistent with our findings, Dalewski et al have found that ESR1 rs1643821 polymorphism is positively associated with anterior disk displacement without reduction, in Caucasian patients 18. Most studies related to the ESR1 gene had evaluated two polymorphic loci in intron 1, known as the XbaI and PvuII the loci 23,24 (not assessed in the present study).
Also, ESR1 SNP rs1643821 could be associated with the severe form of TMD. Previous studies have proven the relationship between SNPs of different genes such as ectonucleotide pyrophosphatase/phosphodiesterase 1 (ENPP1) 25 and alpha-actinin-3 (ACTN3) 26 with the TMD prevalence and higher severity of clinical symptoms in people with facial skeletal asymmetry. Also, another study confirmed the interaction between specific polymorphisms of COMT and ESR1 genes with more severe form of TMD 27. Identifying SNPs that predispose people to TMD can play an important role in recommendations to prevent or reduce the severity of the TMD. Among the prevention and treatment methods for TMD, education of self-care instructions is considered a conservative, and effective method to treat TMD patients especially when it is done continuously 28. For example, self-care and eliminating parafunction habits can reduce the risk of TMD in orthodontic patients with certain polymorphisms.
In human joint tissue, both types of estrogen receptors are expressed by chondrocytes, subchondral bone cells, synoviocytes, and ligament fibroblasts. However, alpha receptors in cortical bone and beta receptors in cartilage, cancellous bone, and synovium are maximal 29.
We found significant associations between the homozygous TT genotype and increased risk of TMD in the ESR2 variants. The role of ERβ is not fully understood but there are controversies about the modulatory, inhibitory, or even reciprocal role of ERβ to that of Erα 30. Although two types of estrogen receptors may be expressed in the same tissue, they are not usually expressed on the surface of the same cell type. If this phenomenon occurs in a cell, ESR-β is usually an antagonist of ESR-α activity 29. It is established that the co-expression of ERα and ERβ overlap in the same brain cells considerably 31. In the present study, this contradictory function of these two receptors is also remarkable. ESR1 A/A homozygosity and A/G heterozygosity were associated with increased relative risk for TMD (Odds Ratio, 4.80, 2.98), but ESR2 T/T homozygosity was associated with decreased risk for TMD (Odds Ratio, 0.41).
Kuchler et al confirmed the presence of ER-α and ER-β receptors in the TMJ tissue of mice, especially young female mice. They also showed polymorphism of ESR1 and ESR2 genes in TMD patients. They reported that ESR2 polymorphism was associated with disc displacement and could be a genetic marker in women with TMD 17. Quinelato et al in 2017, evaluated the association between ER-β and ER-α gene polymorphisms and TMD in Brazilian patients. They reported that the ER-α gene was significantly associated with muscular and articular TMD 29.
Although our results indicate a relationship between COMT SNP rs4680 and the risk of TMD, this relationship was not significant, although allele A in the dominant inheritance pattern can be susceptible to TMD. This might be due to the small sample size. Mladenovic et al in a study with 90 TMD patients and 92 healthy participants, indicated that there was no association between rs4680 and TMD 32. Furthermore, our findings agree with Diatchenko et al in failing to find any evidence indicating an association of the COMT gene (rs4680) with TMD 3. It is important to know that environmental events such as emotional and physical stress, injury, and/or inflammation modify the influence of COMT and ESRs polymorphisms on COMT enzymatic activity 33. Therefore, future studies are necessary to evaluate the effects of environmental non-genetic factors on COMT activity and related phenotypes.
Conclusion :
Our results suggest that ESR1 and ESR2 are involved in the overall risk for TMD. Also, we add to evidence that various genotypes of COMT rs4680 were not statistically different between case and control, but allele A in the dominant inheritance pattern can be susceptible to TMD. It seems that SNPs of ESR1 rs1643821 have a susceptible role and ESR2 rs1676303 has a protective role against TMD.
Acknowledgement :
The authors thank the Technology Development and Industry Relations Management Center of the Tehran University of Medical Science for their excellent technical and financial support. GRANT Number: 9223102008. The study protocol was approved by the Medical Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.DENTISTRY.REC.1397. 056).
Conflict of Interest :
There is not any competing interests in this study.
Funding: This study funded by Technology Development and Industry Relations Management Center of the Tehran University of Medical Science. The authors have no conflict of interest to declare.
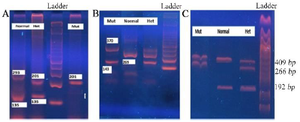
Figure 1. Agarose gel electrophoresis for each T-ARMS-PCR. A) T-ARMS–PCR assay for COMT rs4680, B) T-ARMS–PCR assay for ESR1 rs1643821, C) T-ARMS–PCR assay for ESR2 rs1676303.
|
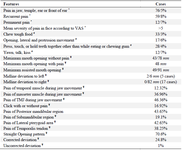
Table 1. Clinical characteristics of TMD patients (n=100)
TMD: Temporomandibular Disorder, VAS: Visual Analogue Scale.
* In the last month, # The pain gets worse during …, ¥ The average of related item.
|
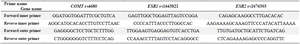
Table 2. PCR primers of COMT, ESR1, and ESR2 genes
|

Table 3. The allelic frequencies of COMT rs4680, ESR1 rs1643821, and ESR2 rs1676303 in the TMD (n=100) and healthy groups (n=103)
wt = wild type, het = heterozygous, mut = mutant, OR = adds ratio, 95%CI = 95% confident interval, Ref = referent genotype.
* Fisher exact test, **chi-square test.
|
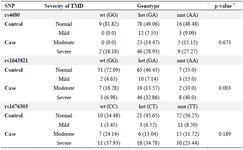
Table 4. Association of rs4680, rs1643821, and rs1676303 with severity of TMD
* Fisher exact test.
|

Table 5. Relationship between TMD severity and related risk factors
Significant values are presented in bold, Categories are created based on a study by Schiffman et al 22.
ϯ student t-test, * Fisher exact test, ** chi-square test.
|
|